The Role of MRI in Neuro-Oncology
Magnetic Resonance Imaging (MRI) is the primary imaging modality in neuro-oncology and plays a central role in the diagnosis, treatment planning, and follow-up of brain and spinal cord tumors. Its ability to provide detailed images of soft tissue makes MRI essential for understanding tumor location, extent, and biological behavior.
What Is an MRI Scan and How Is It Different from CT?
An MRI scan uses strong magnetic fields and radio waves to create high-resolution images of the brain and spinal cord. Unlike CT scans, MRI does not use ionizing radiation, making it suitable for repeated imaging and long-term follow-up.
Compared with CT, MRI offers:
-
Superior visualization of soft tissues, including brain, spinal cord, and nerves
-
Better differentiation between tumor, edema, and healthy tissue
-
Advanced imaging sequences that provide functional and biological information
While CT is often used in emergency settings, MRI is the preferred tool for detailed neuro-oncological assessment.
When MRI Is the Method of Choice
MRI is the imaging method of choice for most suspected or known brain and spinal tumors. It is commonly used to:
-
Detect and characterize primary brain tumors such as gliomas and meningiomas
-
Evaluate spinal cord tumors and nerve involvement
-
Define tumor boundaries for surgical planning and navigation
-
Monitor treatment response and tumor recurrence
-
Assess postoperative changes and radiation effects
Specialized MRI techniques—including contrast-enhanced MRI, diffusion-weighted imaging (DWI), perfusion imaging, and spectroscopy—provide valuable insight into tumor aggressiveness and biological behavior.
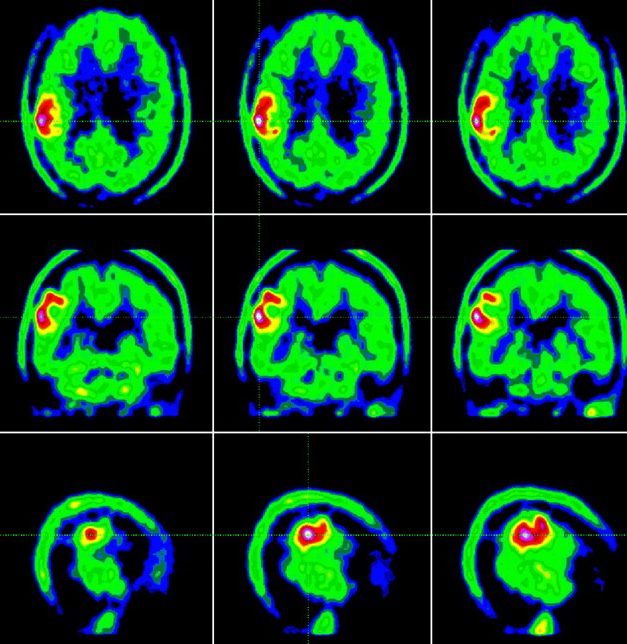
MRI Compared with PET-CT
MRI focuses on anatomical and structural detail, while PET-CT evaluates tumor metabolism and activity. In neuro-oncology:
-
MRI is typically used as the first-line and follow-up imaging modality
-
PET-CT is reserved for specific situations, such as distinguishing tumor recurrence from treatment-related changes or assessing unclear findings
The two modalities are often complementary, with MRI providing precise structural information and PET-CT adding metabolic data when needed.
Why Expert Interpretation Matters
High-quality imaging alone is not enough — accurate diagnosis depends on expert interpretation. An experienced neuroradiologist can identify subtle imaging features that may not be immediately obvious but are critical for correct diagnosis and treatment planning.
For example, on an MRI scan, treatment-related changes after radiation therapy can closely resemble tumor recurrence. A trained specialist can recognize specific imaging patterns and use advanced MRI sequences to distinguish between these possibilities, helping to avoid unnecessary surgery or changes in therapy.
Close collaboration between neuroradiologists and clinical specialists—such as neurosurgeons, neurologists, and neuro-oncologists—further enhances accuracy. By interpreting imaging findings in the context of the patient’s symptoms, medical history, and prior treatments, the care team can make more informed decisions and develop a personalized treatment strategy that best supports patient safety and outcomes.
Conclusion
MRI is the cornerstone of imaging in neuro-oncology. Its unmatched soft-tissue detail and advanced imaging capabilities make it indispensable for diagnosis, treatment planning, and long-term monitoring of brain and spinal tumors. When combined with expert radiological evaluation and multidisciplinary clinical care, MRI supports accurate diagnosis, safer interventions, and improved patient outcomes.
The article was medically reviewed by the Neuro-Oncology Team
Last update: December 14, 2025
Neuro-oncology Institute, Barcelona.