Meningioma: Symptoms, Diagnosis, and Treatment
Introduction
Meningiomas are among the most common primary brain tumors, affecting thousands of people each year. Although most meningiomas are benign (non-cancerous), their size and location can still lead to significant neurological problems. Neurosurgery plays a central role in treatment when symptoms develop or the tumor shows growth. This article explains what a meningioma is, its symptoms, how it is diagnosed, available treatment options, and what patients can expect during recovery.
What Is a Meningioma?
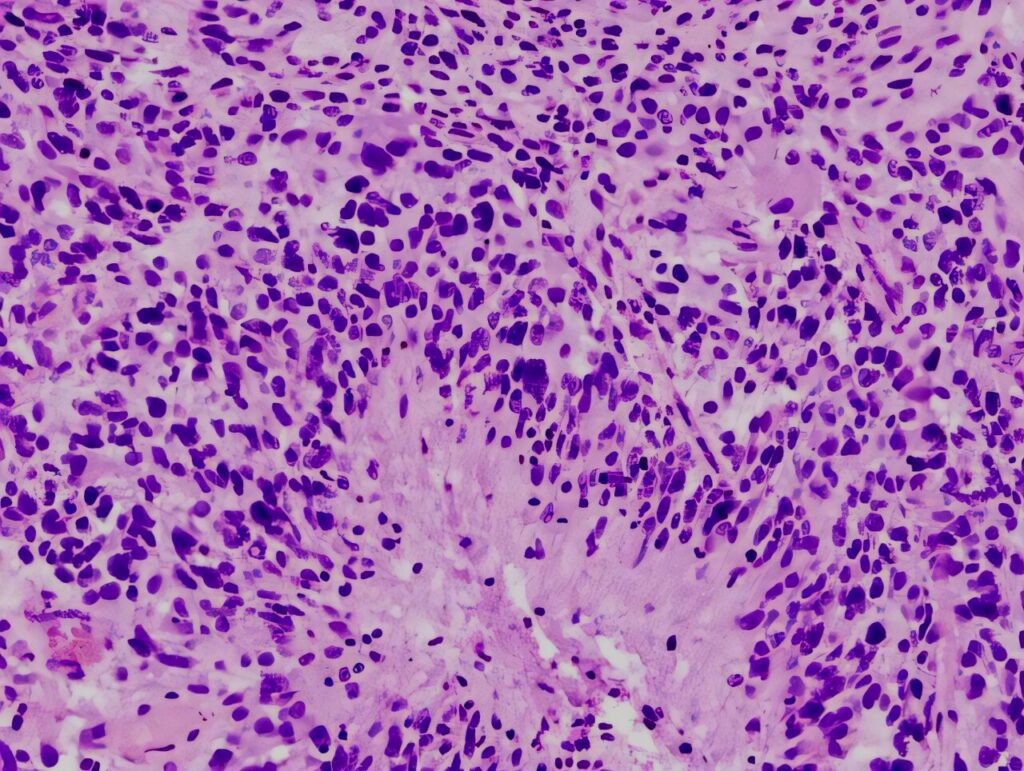
A meningioma is a tumor that arises from the meninges—the protective membranes surrounding the brain and spinal cord. Most meningiomas grow slowly and are benign, but approximately 1–3% are malignant and behave more aggressively.
Key facts about meningiomas:
-
Location: Most develop near the surface of the brain; some occur along the spinal cord
-
Growth rate: Typically slow-growing, often over many years
-
Clinical impact: Even benign tumors can cause serious symptoms if they compress critical brain structures
Because meningiomas originate from the meninges rather than brain tissue itself, surgical removal is often feasible and effective.
Meningioma Symptoms: When to See a Doctor
Many meningiomas are discovered incidentally during imaging performed for other reasons. When symptoms occur, they depend on the tumor’s size, location, and growth rate.
Common symptoms include:
-
Persistent or worsening headaches, often more noticeable in the morning
-
Seizures
-
Vision problems, including blurred or double vision
-
Weakness or numbness in the arms or legs
-
Memory, concentration, or cognitive difficulties
-
Personality or behavioral changes (less common)
When to seek medical attention:
New or progressive neurological symptoms—such as seizures, vision loss, or weakness—should be evaluated promptly. Early diagnosis supports safer treatment and better outcomes.
How Is a Meningioma Diagnosed?
Diagnosis typically involves clinical assessment and imaging studies.
A neurological examination evaluates reflexes, muscle strength, coordination, sensation, and vision.
Imaging studies include:
-
MRI (Magnetic Resonance Imaging): The gold standard for detecting and characterizing meningiomas
-
CT scan: Useful when MRI is unavailable or to assess bone involvement
-
Angiography: Occasionally used to evaluate the tumor’s blood supply
In most cases, imaging findings are sufficient. A biopsy may be performed if tumor behavior or grade is uncertain.
Meningioma Treatment Options
Treatment decisions are individualized and based on tumor size, location, symptoms, growth rate, and the patient’s overall health.
Observation (watchful waiting):
Small, asymptomatic meningiomas may be monitored with periodic MRI scans. Treatment is initiated if the tumor grows or symptoms develop.
Surgery (primary treatment for symptomatic tumors):
The goal of surgery is maximal safe tumor removal while preserving neurological function.
Surgical approaches may include craniotomy, minimally invasive techniques for select tumors, or endoscopic surgery for meningiomas near the skull base.
Potential risks include infection, bleeding, brain swelling, neurological deficits, and tumor recurrence if complete removal is not possible.
Radiation therapy:
Radiation therapy may be recommended when complete surgical removal cannot be achieved, when the tumor is malignant or recurrent, or when surgery presents high risk.
Radiation options include:
-
Stereotactic radiosurgery (SRS), such as Gamma Knife, which delivers highly focused radiation to small, well-defined tumors
-
Fractionated radiation therapy, delivered over multiple sessions for larger or complex tumors
-
Proton therapy, an advanced radiation technique that uses protons rather than X-rays, allowing precise tumor targeting while minimizing radiation exposure to surrounding healthy brain tissue
Proton therapy is especially beneficial for tumors near critical structures, such as the optic nerves or brainstem, and may reduce long-term side effects while maintaining effective tumor control.
Prognosis and Success Rates
With appropriate treatment, outcomes for meningioma patients are generally favorable.
Benign meningiomas have long-term control rates of approximately 80–90% following complete surgical removal. Atypical and malignant meningiomas carry a higher risk of recurrence and often require additional treatment such as radiation therapy. Recurrence rates range from about 10–20% for benign tumors and are higher for aggressive subtypes.
Prognosis depends on tumor location, extent of resection, tumor grade, and the patient’s age and overall health.
Follow-Up Care After Treatment
Long-term monitoring is essential even after successful treatment.
Follow-up care typically includes regular MRI scans—initially every 6–12 months—monitoring for new neurological symptoms, and rehabilitation therapies such as physical, occupational, or speech therapy if needed. Long-term care may also involve managing the effects of radiation therapy and supporting neurological recovery.
Conclusion
Meningiomas are usually benign and slow-growing, but they can significantly affect quality of life if left untreated. Neurosurgery remains the most effective treatment for symptomatic tumors, supported by advanced radiation therapies when needed. Early diagnosis, individualized treatment planning, and consistent follow-up care are key to long-term control.
If you or a loved one experiences persistent headaches, seizures, or neurological changes, prompt evaluation by a specialist is essential. With modern diagnostic tools and treatment options—including precision surgery and advanced radiation techniques such as proton therapy—most patients with meningioma can achieve excellent outcomes and return to active lives.
The article was medically reviewed by the Neuro-Oncology Team
Last update: December 14, 2025
Neuro-oncology Institute, Barcelona.