Diffuse Astrocytoma: Symptoms, Diagnosis, and Treatment
Introduction
Diffuse astrocytoma is a primary tumor of the central nervous system arising from astrocytic glial cells. It belongs to the group of infiltrative gliomas and is characterized by slow to moderate growth, diffuse infiltration of surrounding brain tissue, and a variable clinical course. In contrast to high-grade astrocytic tumors, diffuse astrocytomas generally demonstrate lower biological aggressiveness, although they retain the potential for progression over time.
This article provides an objective overview of diffuse astrocytoma, including its biological characteristics, clinical presentation, diagnostic principles, and current treatment approaches, based on contemporary standards in neurooncology.
What Is Diffuse Astrocytoma?
Diffuse astrocytoma is an infiltrative astrocytic tumor traditionally classified as World Health Organization (WHO) grade 2. In the current WHO classification of tumors of the central nervous system, diffuse astrocytomas are defined primarily by their molecular profile, particularly the presence of an IDH mutation.
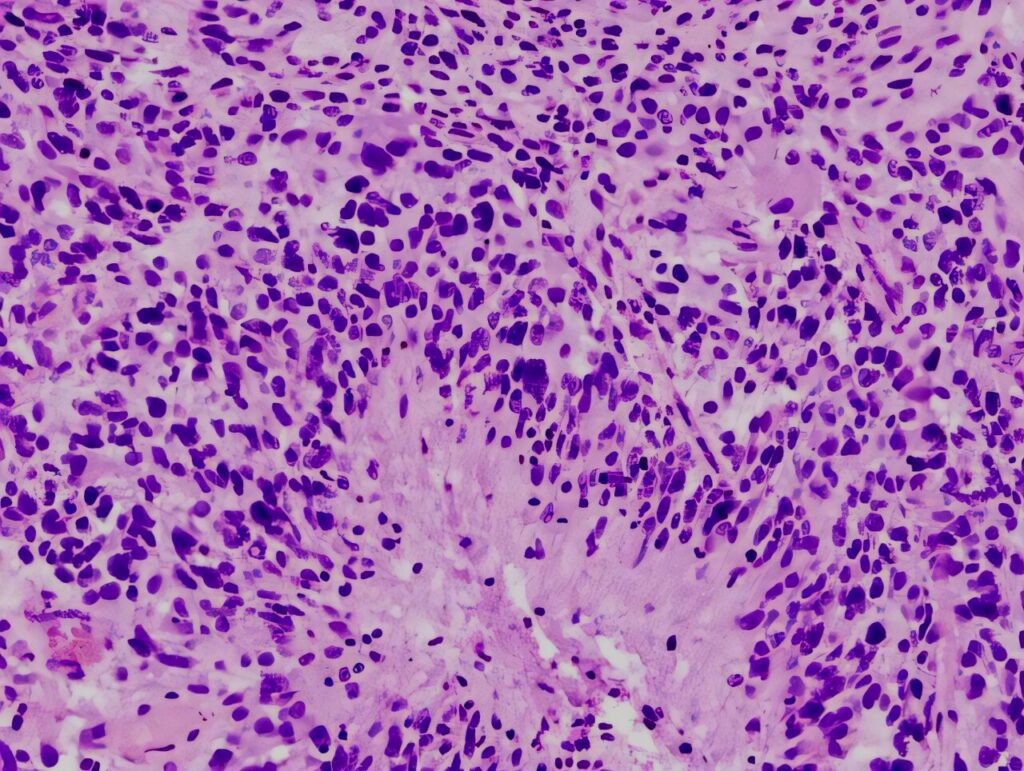
Histologically, diffuse astrocytomas show increased cellularity and nuclear atypia but lack the defining features of higher-grade tumors, such as necrosis or microvascular proliferation. The tumor cells infiltrate normal brain tissue, making complete surgical removal challenging.
Diffuse astrocytomas most commonly occur in young and middle-aged adults and are typically located in the cerebral hemispheres, especially the frontal and temporal lobes.
Causes and Risk Factors
The precise cause of diffuse astrocytoma is not fully understood. Most cases occur sporadically and are not associated with identifiable environmental or lifestyle factors.
Recognized risk factors include increasing age and rare genetic cancer predisposition syndromes. Prior exposure to ionizing radiation involving the brain has been associated with an increased risk of glioma development, although this remains uncommon.
At the molecular level, diffuse astrocytomas are driven by early genetic alterations that affect cellular metabolism and growth regulation, most notably mutations in the IDH gene. These molecular features play a central role in tumor classification and prognosis.
Symptoms of Diffuse Astrocytoma
Symptoms of diffuse astrocytoma develop gradually and are often present for months or years before diagnosis. Clinical manifestations depend on tumor location, size, and degree of infiltration.
Common symptoms include headaches, seizures (frequently the initial presenting symptom), cognitive or memory difficulties, and subtle changes in behavior or personality. Focal neurological deficits may occur when tumors involve functionally critical brain regions.
Compared with higher-grade gliomas, symptom progression in diffuse astrocytoma is typically slower, although neurological deterioration can still occur due to tumor growth or associated brain edema.
Diagnosis of Diffuse Astrocytoma
Diagnosis relies on the integration of clinical findings, neuroimaging, histopathological evaluation, and molecular analysis.
Magnetic resonance imaging (MRI) is the primary diagnostic tool. Diffuse astrocytomas typically appear as non–contrast-enhancing or minimally enhancing lesions, often hyperintense on T2-weighted and FLAIR sequences. Mass effect and surrounding edema are usually less pronounced than in higher-grade tumors.
Definitive diagnosis requires histological examination of tumor tissue obtained through surgical resection or stereotactic biopsy. Histopathology confirms astrocytic lineage and excludes features associated with higher tumor grades.
Molecular profiling is essential for classification and prognostication. Key molecular markers include IDH mutation status, ATRX loss, and TP53 mutations. These features distinguish diffuse astrocytoma from other glioma subtypes and guide clinical management.
Treatment Options for Diffuse Astrocytoma
Management of diffuse astrocytoma is individualized and depends on tumor location, patient age, neurological status, and molecular characteristics.
-
Neurosurgery
Surgical resection is often the initial treatment when feasible. The goals of surgery include maximal safe tumor removal, symptom relief, and acquisition of tissue for histological and molecular analysis.
Because diffuse astrocytomas infiltrate surrounding brain tissue, complete resection is frequently not achievable. The extent of resection must be balanced against the risk of neurological impairment, particularly when tumors involve eloquent brain areas.
-
Radiation Therapy
Radiation therapy may be incorporated into the management of diffuse astrocytoma in selected clinical situations, including tumor progression, residual disease following surgery, or the presence of higher-risk features based on clinical or molecular factors. The decision to initiate radiation therapy, as well as its timing, is individualized and may vary depending on patient age, neurological status, and long-term management considerations.
Conventional fractionated external beam radiation therapy remains the most commonly used approach. Modern planning techniques, such as intensity-modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT), are employed to optimize dose distribution while limiting radiation exposure to surrounding healthy brain tissue.
Proton therapy may be considered in selected cases, particularly when reduction of radiation dose to adjacent normal brain structures is a priority.
Regardless of the modality used, radiation therapy planning in diffuse astrocytoma aims to balance effective disease control with preservation of neurological function, given the typically prolonged clinical course of the disease.
-
Systemic Therapy
Systemic treatment options may include chemotherapy, depending on clinical and molecular factors. Alkylating agents are commonly used when systemic therapy is indicated.
The role and timing of systemic treatment are determined on a case-by-case basis, reflecting the variable clinical behavior of diffuse astrocytoma.
-
Long-Term Management and Surveillance
Given the potential for slow progression and malignant transformation, long-term follow-up with regular clinical assessment and imaging is an essential component of management.
How Diffuse Astrocytoma Differs from Glioblastoma
Diffuse astrocytoma and glioblastoma are both astrocytic tumors, but they differ fundamentally in biological behavior, molecular features, and clinical course.
Diffuse astrocytoma is a lower-grade, IDH-mutant tumor characterized by slower growth and longer overall survival. In contrast, glioblastoma is a WHO grade 4 astrocytic tumor, typically IDH-wildtype, with rapid progression, extensive necrosis, and marked microvascular proliferation.
Imaging features also differ: diffuse astrocytomas often show minimal or no contrast enhancement, whereas glioblastomas typically demonstrate ring-enhancing lesions with central necrosis and significant surrounding edema.
Clinically, diffuse astrocytoma may remain stable for extended periods but carries a risk of progression to higher-grade disease over time. Glioblastoma, by contrast, presents with aggressive clinical behavior from the outset.
These distinctions are critical for diagnosis, treatment planning, and prognostic assessment.
Prognosis and Factors Influencing Outcomes
Diffuse astrocytoma generally has a more favorable prognosis than higher-grade astrocytic tumors, although outcomes vary widely among individuals.
Prognostic factors include patient age, extent of surgical resection, tumor location, and molecular profile, particularly IDH mutation status. Long-term survival is possible, but continued monitoring is necessary due to the risk of progression or transformation.
Conclusion
Diffuse astrocytoma is an infiltrative astrocytic tumor with a variable but often prolonged clinical course. Accurate diagnosis requires integration of histological and molecular data, and management is individualized based on tumor characteristics and patient factors.
Ongoing advances in molecular classification and neurooncology continue to refine diagnostic criteria and inform treatment strategies, supporting more precise and personalized care.
The article was medically reviewed by the Neuro-Oncology Team
Last update: January 4, 2026
Neuro-oncology Institute, Barcelona.